Abstract
Background
Hemophagocytic lymphohistiocytosis (HLH) is a rare syndrome characterized by a state of hyperinflammation and associated with poor outcomes. It is primarily driven by macrophages and T-cells leading to unregulated cytokine release, tissue infiltration, and multisystem failure. The HLH 2004 study listed the widely accepted diagnostic model which requires the presence of 5 out of 8 criteria (Fever; splenomegaly; bicytopenia; hypertriglyceridemia or hypofibrinogenemia; hemophagocytosis, ferritin >500 mcg/L; Low/absent NK-cell activity; soluble CD25 elevation). The current management guidelines based on HLH-94 studies involve immunosuppression with weekly chemotherapy (etoposide) and glucocorticoids (dexamethasone), intrathecal methotrexate is administered in patients with CNS involvement. Our objectives were to review management guidelines of HLH and clinical outcomes at the University of South Alabama health system.
Method:
We conducted a retrospective observational single site study for both adults and pediatric cases of HLH. The electronic medical records of eligible patients diagnosed with HLH, based on HLH 2004 criteria meeting 5 out of 8, were reviewed. Demographic and clinical outcomes data from the subjects were collected from the chart review. Statistical analysis for the baseline patient characteristics presented as the mean ± standard deviation for continuous variables. Categorical variables were described using frequency counts and percentages.
Results
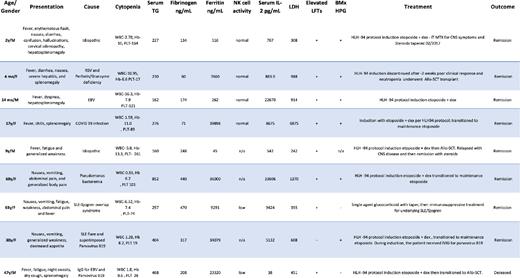
All nine patients included in this study met criteria for HLH as defined in the HLH 2004 study. The median age at diagnosis was 17 (range 1-69 years) with a female predominance of 3:2. Two out of nine (22%) patients had been on immunosuppressive therapy prior to diagnosis; one on maintenance prednisone for SLE, and the other on dexamethasone for intracranial tumor. Laboratory features are summarized in table 1. The peak median ferritin was 9,291 ng/mL (range 45-39,898 ng/mL). The sIL2R at diagnosis ranged from 38-33,606 pg/mL (reference <1,100 pg/mL). Patient clinical manifestations are summarized in Table 2 and 3. All patients presented with fevers and cytopenias. Five (55%) demonstrated splenomegaly and seven (78%) patients had evidence of hemophagocytosis in the bone marrow. Seven patients (78%) had secondary HLH due to infection, one patient (11%) had an underlying malignancy with the remaining case being idiopathic. Seven patients received etoposide and dexamethasone per HLH-94, one patient received stem cell transplantation, and the remaining patient received glucocorticoid with taper. At the time of this report, eight of nine (89%) patients were still alive. Interestingly, the deceased patient was one of only two patients in our series with extremely low or absent NK-cell activity. Univariate analysis for age, triglyceride, and IL-2 levels are associated with higher length of stay in the hospital.
Discussion
Most cases of primary HLH are sporadic in nature with a genetic familial predisposition. The secondary causes of HLH include autoimmune disorders, infectious diseases, immunodeficiency syndromes, and hematologic malignancies. In this study, infection was the predominant cause of HLH in both adults and children. This differs from previous studies which suggested that adult HLH was more commonly associated with malignancy. We found 2 patients with autoimmune conditions on immunosuppressive therapy. Diagnosis of HLH remains a challenge due to variability of clinical presentation and lack of specificity of laboratory findings. The current diagnostic criteria from HLH 2004 was not designed for adult HLH. Treatment is often delayed due to the turnaround of specialized labs and under recognition of this disease. Optimizing diagnostic criteria for earlier detection may benefit both children and adults. Experience with novel agents such as JAK inhibitors and anti-IL-6 during covid pandemic or with T-cell cellular therapies to control the cytokine storms would be an interesting target to study their efficacy in HLH prospectively.
Disclosures
Alkharabsheh:AstraZeneca: Consultancy; Incyte: Consultancy; Genentech: Consultancy; Agios: Consultancy; Amgen: Consultancy; National Community Oncology Dispensing Association, Inc: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal